Now What? Life Beyond Your Visit
Top 12 Next Steps, FAQ, and Resources for Your JourneyA care navigator for patients, families, and care partners

Welcome to The Memory Center at UChicago Medicine!
You are not alone, and it can be overwhelming to imagine where to start.
No matter where you are in your journey, the more you learn, the earlier you start,
the more confident and equipped you can be in managing your care.
Here are the most frequently asked questions regarding support, resources, and next steps.
Explore these as often as needed. Whether you are the patient, a care partner, family member, concerned friend or neighbor, these resources may be helpful along the way.
Visit this space after your first appointment. Come back again throughout your journey.
Learn as much as you can, so everyone involved can have more rest and enhanced quality of life!
New to care planning?
Peruse these top 12 common topics below, and if you want more guidance, feel free to refer to the PDF accessible guides, videos, and links located throughout, and especially at the bottom of this page, in addition to in-person opportunities to connect for personalized care planning.
Start Here
Be prepared for every visit with your doctor.
Reviewing an Activities of Daily Living Checklist in advance of each appointment.
(It can help to print the above checklist or jot down notes to bring, to help make your clinic visit efficient,
and so that the medical team can assist in the diagnosis and treatment plan as accurately as possible.)
Then after your visit, explore the below tips, resources, and support options to guide you as often as needed.
Table of Contents
- Learn More
- Keep up with Your Medical Appointments
- Find Support in & Out of Home
- Plan Ahead NOW: Legal, Financial, & Long-Term Care Planning
- Tips, Tools, & Treatments Beyond Your Visit
- Safety: At Home & on the Road
- Exploring Clinical Research Studies & Medical Treatment
- Lifestyle, Wellness, & Quality of Life
- Living Alone
- For Those Who are Working
- For Those Under 65 (Young Onset)
- How can we help the cause?
Grief and Loss Support can Happen Now
Where else can I receive individualized support and resources for care planning through this journey?
(PDF Guides, Videos, Resource Toolkits, 1:1 Care Planning Consultations)
1. Learn More
First, learn as much as you can.
No matter where you are in your journey, the more you learn, the earlier you start, the more confident and equipped you can be in managing your care — from diagnosis education and communication strategies, to resources for enhancing quality of life for everyone involved.
In this section:
– What if I don’t have a diagnosis yet?
– What’s dementia? Alzheimer’s? Other diagnoses? Where can I learn more?
– Coping, adjusting, and handling tough communication and behaviors
– Important considerations for those with cognitive impairment going into surgery with anesthesia (Questions to ask your surgery team / anesthetist)
Q: I don't have a diagnosis yet or am in the middle of a workup. Is it ok to learn more now?
A: It is important to confirm your diagnosis with a neurologist first, rather than guessing or searching online in advance. Not to worry, we treat the symptoms in the meantime, and you can acquire support for your overarching daily needs from any of these broader sites and resources below.
For now, peruse and use this information most especially related to assisting with your daily care needs and for tips in responding to specific challenges and behaviors.
As for the specific diagnosis and medical treatment plan, we recommend confirming your diagnosis or completing your workup before you start reaching out to any particular organization for support related to that diagnosis. Once you have a diagnosis, then you can learn about the various types of dementia below and get connected to your local association that supports your specific condition.
Q: What is Dementia vs. Alzheimer’s Disease and other related diagnoses? Where can I learn more? What are the national organizations that support my condition?
A: “Dementia is not a specific disease. It’s an overall term that describes a wide range of symptoms associated with a decline in memory or other thinking skills severe enough to reduce a person’s ability to perform everyday activities. Alzheimer’s disease is the most common type of dementia and accounts for 60 to 80 percent of cases. Other types of dementia include Dementia with Lewy Bodies, Frontotemporal, and Vascular [and more, as seen below].” – Dementia Friends USA
These sites cover information on Alzheimer’s Disease and all other related dementias. Explore to learn what to expect along the way.
The Memory Center at UChicago Medicine
See a brief description of all the various types here | About Dementia
NIA: National Institute on Aging | Alzheimer’s Disease and Related Dementias
www.nia.nih.gov/health/alzheimers
Alzheimer’s and related Dementias Education and Referral (ADEAR Center) | www.alzheimers.gov | 800-438-4380
Alzheimer’s Association | www.alz.org | 800-272-3900 (24/7 helpline)
Alzheimer’s Foundation of America | www.alzfdn.org | 866-232-8484
Alzheimer’s Disease International | https://www.alzint.org/ –
_____________________________________________
Once your specific diagnosis is confirmed, if you have any of the other related dementias, connect with your local chapter of the association connected to your condition:
Alzheimer’s Association (covers all types of dementias) | www.alz.org | 24/7 helpline 800-272-3900
Alzheimer’s Disease Education and Referral Center | www.nia.nih.gov/Alzheimer’s | 800-438-4380
Alzheimer’s Foundation of America | www.alzfdn.org | 866-232-8484
Lewy Body Dementia Association | www.lbda.org | 800-539-9767
The Association for Frontotemporal Degeneration | www.theaftd.org | 866-507-7222
American Parkinson Disease Association | www.apdaparkinson.org | 800-223-2732
Creutzfeldt-Jakob Disease Foundation Inc. | www.cjdfoundation.org | 800-659-1991
CurePSP (including FTD, PSP, and CBD) | www.psp.org | 800-457-4777
Huntington’s Disease Society of America | www.hdsa.org | 800-345-4372
Hydrocephalus Association (NPH) | www.hydroassoc.org | 888-598-3789
Posterior Cortical Atrophy (PCA) | Korsakoff syndrome | Down syndrome | Vascular dementia:
Please refer to www.alz.org and www.dementiasociety.org for more information/support on the conditions above.
These resources can also be found on our page at: https://thememorycenter.uchicago.edu/resources-links/
Q: Where can I learn more about memory loss and how to adjust to this new diagnosis? Can I learn how to handle tough communication and behaviors prior to a diagnosis?
It is never too early to learn how to interact with compassion and dignity through mild cognitive impairment and dementia. Disagreements and escalated or heated moments may arise. Here’s how to keep things cool and calm, regardless of knowing your diagnosis.
START HERE: COMMUNICATION STRATEGIES
We recommend that ALL patient’s families and care partners receive an introduction to Communication Strategies (1st 30 min = Alzheimer’s Association; 2nd 30 min = from The Memory Center). Visit often, pause, take notes, watch in segments, and replay anytime. This will help the person with memory loss feel seen, heard, safe, and de-escalated. It will also enhance smoother interactions on a daily basis.
HOW AND WHEN DO I SHARE THE NEWS? – Sharing a Dementia Diagnosis with Family and Friends – a guide presented by Alzheimer’s Texas, for Alzheimer’s Disease and related disorders
How do I plan ahead? What do I need to consider for my care needs along the way? Peruse the topics below, and they outline all that you need to explore. For personalized guidance, see below, which provides PDF guides, videos, care navigation websites, and toolkits at your fingertips. At the very bottom of this page, you can find additional opportunities for free 1:1 care planning consultations.
CARE PLANNING GUIDES:
Our team members have contributed to the development and creation of this comprehensive care planning resource guide: ‘Centering Our Values’ curated by SHARE Network Chicago, our very own HRSA grant funded initiative within the UChicago Medicine Geriatrics and Palliative Care Section. Visit here: https://centeringourvalues.org/
‘Pathways to Well-Being’ – https://daanow.org/pathways-to-well-being-with-dementia/
Dementia Unplugged – View this series of videos from the Dementia Society of America – https://www.youtube.com/playlist?list=PLoyKaLxoKOcWxh-uIUtAvid4avZ5d31xj
CREATE A DAILY CARE PLAN:
https://www.alz.org/help-support/caregiving/daily-care/daily-care-plan
RESPONDING TO CHALLENGING MOMENTS AND BEHAVIORS:
Teepa Snow – is world famous for her wit and compassion. Visit this archive of videos that help you respond to every possible situation that can arise through cognitive impairment or in dementia care. https://www.youtube.com/channel/UCSXrEX7LkWOmfTaV6u1C7wQ
www.teepasnow.com
Additional On Demand Recordings:
https://www.alz.org/illinois/helping_you/education/virtual_learning
Helpful Digital Publications:
https://www.alz.org/help-support/resources/publications
Become a ‘Dementia Friend’! Learn how to notice dementia in your community. Watch these brief videos to see how to help in a store, library, church, dining, medical setting, and more. Once viewed, you are officially added to the national count as a ‘Dementia Friend’! You can spread the word to others and contribute towards this nationwide effort to increase awareness.
https://dementiafriendsusa.org/
Q: What are some recommended books and podcasts?
◾Loving Someone Who Has Dementia: How to Find Hope while Coping with Stress and Grief, by Pauline Boss, PhD
◾The Busy Caregiver’s Guide to Advanced Alzheimer’s Disease, by Jennifer Stelter, PsyD (https://www.dementiaconnectioninstitute.org/resources)
◾ The 36-Hour Day: A Family Guide to Caring for People Who have Alzheimer’s Disease,Related Dementias and Memory Loss, 5th ed., by N. Mace, MA and P. Rabins, MD, MPH
◾ Learning to Speak Alzheimer’s: A Groundbreaking Approach for Everyone Dealing with the Disease, by J. K. Coste & R. Butler
◾ Creating Moments of Joy for the Person with Alzheimer’s or Dementia, by Jolene Brackey (www.enhancedmoments.com)
◾ Coping with Alzheimers: A Caregiver’s Emotional Survival Guide, 4th ed., by Rose Oliver PhD & Frances Bock, PhD
◾ To Survive Caregiving: A Daughter’s Experience, A Doctor’s Advice
by Cheryl Woodson, MD
◾ We Danced, by Scott Rose
◾ A Guide for Recalling & Telling your Life Story by Hospice Foundation
◾ The 24-Hour Rule: Living with Alzheimer’s, by Cheryl Levin-Folio
◾ The Neuroscience of Memory: Seven Skills to Optimize Your Brain Power, Improve Memory, and Stay Sharp at Any Age, by Sherrie D. All, PhD.
◾ Don’t Toss My Memories in The Trash, by Vickie Dellaquila
◾ Alzheimer’s Early Stages, by Dan Kuhn, MSW
◾Dementia Reconsidered, Revisited: The Person Still Comes First, by Tom Kitwood
◾A Personal Guide to Living with Progressive Memory Loss, by Sandy Burgener and Prudence Twigg
◾Mom, Are You There? Finding a Path to Peace through Alzheimer’s, by Kathleen Negri
◾Younger People with Dementia, by Sylvia Cox and John Keady
◾The Complete Guide to Alzheimer’s Proofing Your Home, by Mark and Ellen Warner
◾Still Alice, by Lisa Genova
◾The Person with Alzheimer’s Disease: Pathways to Understanding the Experience, by Phyllis Braudy Harris
◾Alzheimer’s from the Inside Out, by Richard Taylor
◾Comforting the Confused: Strategies for Managing Dementia, by Stephanie Hoffman and Constance Platt
◾Don’t Forget by Jane Godwin
◾The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s and Other Dementias, by Naomi Fell
◾Forget Memory: Creating Better Lives for People with Dementia, by Anne Davis Basting
◾What’s Happening to Grandpa? by Maria Shriver
◾ Alzheimer’s Early Stages: First Steps for Family, Friends, and Caregivers; 3rd Updated Edition, by Daniel Kuhn, MSW
◾ The Art of Dementia Care, by Daniel Kuhn, MSW
◾ The Best Friends Approach to Dementia Care; 2nd edition by David Troxel and Virginia Bell
◾ Alive Inside: Music & Memory [Netflix] Build a personal playlist! www.aliveinside.us
ADDITIONAL BOOK LISTS:
https://ageucate.com/index.php?main_page=books
www.alz.org/library | www.alz.org | www.alzfdn.org
https://www.ypwd.info/shop/books
PODCASTS and FILMS:
◾ Alive Inside (documentary): Music & Memory [Netflix] Build a personal playlist! www.aliveinside.us
◾ Rachel and Maria – Remember Me (podcast): https://www.remembermeftd.com/
◾ Sharon Hall – Talking FTD for You (podcast): https://talkingftd4you.podbean.com/
◾ Lori La Bey – Alzheimer’s Speaks (podcast/site): https://alzheimersspeaks.com/
◾ Pedacito de Carne (short film): https://www.filmindependent.org/programs/fiscal-sponsorship/pedacito-de-carne/
Q: I have surgery coming up. What questions can I ask my anesthesiologist due to my cognitive impairment? (Going under for full anesthesia may create further cognitive impairment and it is important to discuss with your surgery team.)
1. “Given my memory issues, is there anything that can be done to reduce the risk of confusion or memory worsening after surgery?”
2. “Will I be meeting the anesthesiologist before surgery? Can you make sure they’re aware of my cognitive impairment?
3. “Would regional anesthesia or a lighter form of anesthesia be possible for this procedure?” – Is there any way to use spinal or epidural anesthesia for this surgery?”
4. “If general anesthesia is needed, will they use a lighter approach or brain monitor (like BIS) to reduce the chance of confusion afterward?”
5. “Because of my memory concerns, are there any medications we can avoid or adjust to reduce the risk of confusion afterward?”
6. “Do you normally use drugs like Versed (benzos) or scopolamine? If so, is it possible to avoid them in my case?”
7. “How will my pain be managed in a way that avoids heavy opioids or sedating medications?”
8. “Will the anesthesia team be informed about my memory issues before surgery?”
2. Keep up with Your Medical Appointments
We often hear, how long is this condition? How far along am I? The best way to gauge your health is by seeing your doctors regularly (primary care and/or specialists). Explore here for answers and transportation options to UChicago Medicine.
In this section:
– What’s my prognosis? What’s next?
– Transportation to get to your visits
Q: What is the prognosis? How do I know how far along I am? What is next after my first visit?
The journey of an Alzheimer’s or other related dementia can range vastly, from 2 to 10-20 years.
The best marker of progression is keeping up with your medical appointments.
Typically there is a visit about 3 months after diagnostic workup, and every 6 months thereafter, until the doctor indicates you are ready to stretch out to an annual follow up.
You as the observing care partner can know best what stage they are in depending on the symptoms you notice.
For example, use the symptom checker below to on the stages of dementia to gauge the status of progression.
https://www.alz.org/alzheimers-dementia/stages
Between visits, you can contact the clinic for symptom flare-ups, behavioral challenges, obvious changes, and obstacles in care. We can assess for adjustments in medication, increasing level of care needs, and rule out any other underlying health issues (e.g. respiratory or urinary tract infections).
Q: What are my transportation options for getting to my appointments?
- Family, friends, neighbors, faith community, caregivers
– Explore first with your immediate network if you have anyone that can take you to your doctor appointments
- Public transportation
– rideshare: (Uber | Lyft | www.Gogograndparent.com)
– bus/train/taxi: PACE | CTA | Metra | Taxi (www.chicabs.org)
– local neighborhood: inquire with your local area agency about transportation services available in your own neighborhood (www.eldercare.gov)
- Transportation for People with Disabilities
– PACE – $0-2: bus | train | Dial-a-Ride | on-demand | taxi (below)
info/details: https://www.pacebus.com/riders-disabilities
– PACE Taxi Access Program (City of Chicago) – The TAP Program is for PACE eligible riders. Apply for PACE first, then order your TAP Card.
Once you have your TAP card, for only $2 per ride you can buy one-way taxi rides worth up to $30 per ride. You can take up to 8 one-way taxi rides a day! (Regular cabs and wheelchair-accessible cabs available, 24/7, no advance reservations needed)
info/details: https://www.pacebus.com/tap
printable PDF: https://www.pacebus.com/sites/default/files/2023-03/TAP%20User%20Guide.pdf
- For those with MAP Health insurance: Contact your provider to see if you have the benefit that offers up to 10 one-way rides for your medical appointments
- For Medicaid patients: All Medicaid patients have free transportation to all medical appointments; must be reserved at least 3 business days in advance
– Call the number on the back of your insurance
– All first-time users must complete a CTS form – https://www.netspap.com/providers/forms
3. Find Support in and Out of Home
Caregiving should not be done alone. Explore here for support, training, and education. Free, reduced cost, and private pay options exist that help to stretch your dollar and reclaim your time with good rest and balanced quality of life for both the patient and the care partners.
In this section:
– Caregiver Training and Education
– Caregiver Support
– Additional resources (e.g. Awareness Cards, pro-tips in managing care)
– In-Home Care
– Adult Day Centers vs. Senior Centers
– Residential Living options
Q: What caregiver training and education opportunities are out there?
See the bottom section for PDF care planning guides, toolkits, websites, and 1:1 care navigation opportunities!
Here are additional learning and education opportunities for care partners/families:
The Savvy Caregiver Program: https://www.alzheimers-illinois.org/education/savvy-caregiver.asp
Powerful Tools for Caregivers provides online and in person classes for caregivers to take better care of themselves whilst caring for a loved one. Programs available in English, Korean, Spanish and French. https://www.powerfultoolsforcaregivers.org/what-we-do/
Aging Care Connections: Call 708-354-1323 for in-person support groups: https://www.agingcareconnections.org/caregiver-support.html
The Stress Busting Program for Caregivers: Enter location and zip code to find trainings in your area: https://www.wellmedcharitablefoundation.org/caregiver-support/caregiver-stress-busters/for-caregivers/
Family Caregiving Alliance: https://www.caregiver.org/connecting-caregivers/services-by-state/?state=illinois
Caregiver Action Network (CAN): CAN provides education, peer support, and resources to family caregivers across the country free of charge: https://www.caregiveraction.org/
DementiaMap.com is an excellent website including a resource directory, events calendar, glossary and blog.
Alzheimer’s Speaks: A radio show to give people solid information and ideas, raise dementia awareness and connect people around the globe: https://www.blogtalkradio.com/alzheimersspeaks
Being In The Moment is an online resource with short videos to help caregivers navigate every aspect of caregiving for dementia patients: https://beinginthemoment.org/pathways/
Dementia Live is a transformative dementia simulation and empathy training experience that empowers staff, families and the community at large. See ageucate.com, a training institute that leads this program: https://ageucate.com/index.php?main_page=dementia_live
Q: What caregiver support options are out there?
- Toll-free help: 800-272-3900 (alz.org) | 866-232-8484 (alzfdn.org)
Phone-based support group: Sign-up at 866-232-8484 (alzfdn.org)
Online: alzconnected.org | www.caregiving.com | www.caring.com - Caregiver support group: 1st Thursdays | 1-2:30pm | (773) 702-8840 South Shore Senior Center | 7101 S. Exchange Ave. Chicago, IL
SHARE Network runs a Caregiver Support Group on the last Monday of each month via Zoom. Check this link for information: https://sharenetworkchicago.org/events/
Hilarity for Charity is an organization that offers online support groups for caregivers as well as other support programs: https://wearehfc.org/programs/#caregiver-respite-grant
Dementia Connection Institute – Offers creative tips and techniques for helping care partners engage with their person diagnosed through evidence based practices rooted in research, particularly in how to enhance quality of life by engaging with the person’s five senses when the loss of verbal capacity occurs over time. https://www.dementiaconnectioninstitute.org/ (https://www.dementiaconnectioninstitute.org/resources)
Younger / Early Onset Resources (see #11 below as well):
Alzheimer’s Association – www.alz.org/youngeronset
Without Warning: Younger Onset Support Group – screening required www.withoutwarning.net
Lorenzo’s House is an organization designing holistic memory care and support programs for loved ones and their families navigating younger-onset Alzheimer’s: https://lorenzoshouse.org/
Diagnosis-specific support is also available at your respective organization for the name of your diagnosis. They often have helplines and support groups. See #1 above under ‘Where can I learn more?’ for a comprehensive listing of diagnosis-specific dementia care organizations.
Additional support groups for caregivers and patients can be found here:
https://ilbrainhealth.org/support-services/support-services/
https://www.wellmedcharitablefoundation.org/caregiver-support/caregiver-teleconnection/
https://sharenetworkchicago.org/resources/caregiver-support-groups
Q: What else can help with coping and adjusting to this journey?
- Care Planning Session – See the bottom section for care planning guides and in-person/virtual opportunities to learn more and plan ahead for short- and long-term
- Awareness Cards – Signage to communicate to the public can be very helpful. It elicits increased empathy, patience, and compassion.
‘Just A Minute’ (JAM) Cards: The Dementia JAM Card, for people living with dementia/memory problems, is a discreet way of telling people that they may sometimes need a little extra time and patience.
https://www.communityni.org/news/dementia-jam-card
Younger Onset Cards
https://alzheimer.ca/en/about-dementia/other-types-dementia/young-onset-dementia/id-cards
FTD Awareness Cards
https://www.theaftd.org/living-with-ftd/resources/awareness-cards/
- Caregiver’s Guide to Understanding Dementia Behaviors by the Family Caregiver Alliance (www.caregiver.org) (found on www.caregiver.org/print/17)
- caregiving.com has many online articles, resources including webinars and podcasts, for eg. https://www.caregiving.com/posts/tips-for-communicating-with-dementia
- Alzheimer’s Association has a comprehensive caregiver support resource online: https://www.alz.org/help-support/caregiving
- SHARE Network: Focused on the South Side of Chicago, SHARE Network brings older adults, caregivers, primary care providers, and geriatric specialists together to share knowledge and resources. Free transportation is available to educational and social events. https://sharenetworkchicago.org/
- Videos: Interested in building empathy and compassion among care partners, friends and family members? Ask your social worker, a Certified Dementia Communication Specialist, to share brief videos and communication strategies, including how to see the world from the lens of those experiencing memory loss.
–Free series: The Alzheimer’s Project (https://www.hbo.com/documentaries/the-alzheimers-project-caregivers) - Teepa Snow’s website has comprehensive videos, webinars and resources for patients and caregivers including specific ways to support those living with brain changes: https://teepasnow.com/; https://tinyurl.com/t3h3nb8j
- Reading for the one experiencing memory loss:
The By Us For Us series of guides, by the Murray Alzheimer Research and Education Program, created by those with memory loss for those with memory loss. (available for download online: https://the-ria.ca/resources/by-us-for-us-guides/) - Alzheimer’s Association & AARP Community Resource Finder is a database of dementia and aging-related resources that makes it easy for individuals and families to find programs and services in a specific location. https://www.communityresourcefinder.org/
- Coping through various losses and complex situations:
–Loss & Aging (www.griefcounselor.org) Click on ‘Human Potential’
–Family healthcare counseling (www.ccfhchicago.org) 312-372-4731
–Counseling (www.inhomecounselingforseniors.com) 888-903-5604
–Mental health resource/help 312-563-0445 (www.namichicago.org)
– Chicago Center for Cognitive Wellness: Therapists with expertise in memory care and memory loss diagnoses. Dr. Sherrie All is a clinical neurorehabilitation psychologist and brain health expert. http://cogwellness.com/, 773-345-3495, Edgewater and Loop office locations.
- Ask your social worker, a Certified Dementia Communication Specialist for a detailed list of suggested counseling services and providers.
Q: What kind of In-Home Care options do I have?
Caregiving Respite: Assistance for caregivers is available depending on your location. There are several options for coordinating caregiving respite.
- For the city of Chicago – call 312-744-4016 or email aging@cityofchicago.org. Online information: https://www.chicago.gov/content/dam/city/depts/fss/supp_info/SeniorServices/Caregiver/DFSSCaregiverPgmRespiteSvcs.pdf
General overview for Caregiving Assistance: https://www.chicago.gov/city/en/depts/fss/provdrs/senior/svcs/caregiving_assistanceservices.html
2) Chicago suburbs: AgeOptions, https://services.ageoptions.org/ This web page allows you to find your local Care Coordination Unit (CCU), using your home address. Call (708) 383-0258 for assistance.
3) Northeastern Illinois: Contact AgeGuide, https://ageguide.org/family-caregiver-program/ Servicing DuPage, Grundy, Kane, Kankakee, Kendall, Lake, McHenry and Will. Call (800) 528-2000.
4) Beyond Chicago: You can contact www.eldercare.gov for resources in your area, https://eldercare.acl.gov/Public/Index.aspx or call 1-800-677-1116.
For additional options: check out SHARE Network’s guide, https://sharenetworkchicago.org/resources/respite-care#
Q: What is an adult day program? How is this different from a senior center?
Adult Day Centers are for those that can benefit from a structured, secure environment. They can be private pay or subsidized by the state at 1/2 or full day, with affordable rates. This is a common, low-cost option for families that work or for individuals that live alone. Some day centers include transportation, and participants can enjoy meals, recreation, exercise, social opportunities, brain health education, and light assistance with medication administration, often with nurses on staff to care for Activities of Daily Living.
Adult Day Service is designed especially for older adults who cannot be home alone during the day. Adult day service also provides respite for family caregivers.
A helpful resource to explain options can be found here: https://www.alz.org/help-support/caregiving/care-options/adult-day-centers
For Chicago and surrounding areas: Go to https://webapps.illinois.gov/AGE/providerprofilesearch to click on your county (enter zip code) to determine options and to contact your local Care Coordination Unit.
The National Adult Day Services Association has a searchable database by zip code: https://www.nadsa.org/consumers/choosing-a-center/
SHARE Network has a list of Adult Day Care options in Illinois: https://sharenetworkchicago.org/resources/adult-day-care
The Alzheimer’s Association and AARP Community Resource Finder also has a national directory for in-home care and adult day options. Visit www.communityresourcefinder.org > Home Care > Adult Day
www.eldercare.gov – This is the national site for every region’s local Area Agency on Aging, and you can request adult day services
A senior center is open to the public and is available to those who require less care. They often have recreational programming and participants are able to attend with a care partner. These are the local City of Chicago Senior Centers: https://www.chicago.gov/city/en/depts/fss/provdrs/senior/svcs/regional_senior_centers.html
To inquire about your local senior center and other programs, resources, and caregiver support services available to you, visit:
www.ilaging.illinois.gov – Department on Aging – City of Chicago
www.AgeOptions.org – Suburban Cook County
www.AgeGuide.org – Collar Counties (DuPage, Grundy, Kane, Kankakee, Kendall, Lake, McHenry and Will)
www.eldercare.gov – National Website for your local Area Agency on Aging
Q: What residential community living options do I have?
Considering a Move or Transition for Long-Term Care? Your social worker can explore the differences between levels of care: independent-, assisted-, supportive-living, memory care and skilled nursing. This is a change that may require tailored guidance an interdisciplinary approach between your social worker and your medical provider.
Elderwerks: Free senior assistance/referrals for housing and professional services (https://www.elderwerks.org) | 847-877-8215
Senior Living Specialists: https://www.seniorlivingspecialistschicago.com/ | 847-710-3255
For your own search for nursing homes, home health agencies and other medical providers, visit https://www.medicare.gov/care-compare/
For your own search for independent and assisted living, memory care and adult day centers, please visit communityresourcefinder.org
4. Plan Ahead NOW: Legal, Financial, & Long-Term Care Planning
Get ahead of missed bills, ensure you have the right advance directives in place, and the people you trust to assist in your care.
In this section:
– Advance Directives (Power of Attorney of Healthcare and Property)
– Financial planning and Paying Bills
– Elder Law consultation
Q: What do I need to consider and prepare in advance?
– Advance Directives – Identifying your Power of Attorney of Healthcare and Finances is free and does not require an attorney. Speak with your clinic social worker and bank to complete or review the links below.
– Bills/Finances – Explore a financial counseling consultation; Identify someone you trust to assist with managing your bills and finances.
– Elder Law consult – To plan your estate, finances, and budget long-term care in advance
If you prefer an agency to represent you as Power of Attorney or Guardian, your clinic social worker can connect you accordingly.
https://prepareforyourcare.org/en/welcome
5. Tips, Tools, & Treatments Beyond Your Visit
Beyond medical treatment, did you know that you can have insurance-covered therapies to optimize your wellness? Cognitive neuro rehab and memory strategies, individual counseling, physical and occupational therapy all help you keep your brain and body strong.
In this section:
Know the difference. . .
– Cognitive / Communication Therapy, Speech Therapy, Occupational Therapy, and Physical Therapy
– In-Home Care vs. Home Health vs. Outpatient Therapy
Q: What kind of therapies and treatments are available to me beyond the medical clinic visit with my doctor?
Memory loss can impact one’s level of functioning and productivity. Speech and occupational therapy, cognitive memory strategies, environment modifications, and home safety assessments can help enhance quality of life. Sometimes, an adjustment to the living arrangements are needed as well.
MemoryCare Corporation – provides individual ‘person-centered’ therapy for patients and families including speech, occupational therapy, physical therapy as well as cognitive classes, counseling and support. In-person and virtual opportunities for PT/OT/ST (cognitive communication therapy), offered at specific Chicagoland sites and select areas for appointment visits at home. Call (630) 800-2444 for more information. https://memorycarecorp.com/
De Paul Speech Clinic – DePaul has a speech and language therapy clinic in Lincoln Park. They provide speech and language evaluations and cognitive communication therapy to all individuals regardless of their ability to pay for services. Services are offered in English and Spanish. Call (773)325-7040 or email slpclinic@depaul.edu. (A free, donation-based clinic with bilingual services and accessible to all with or without insurance) https://resources.depaul.edu/newsline/sections/campus-and-community/Pages/speech_language_clinic.aspx
(A free, donation-based clinic with bilingual services and accessible to all with or without insurance) https://resources.depaul.edu/newsline/sections/campus-and-community/Pages/speech_language_clinic.aspx
Shirley Ryan Ability Lab – offers intensive outpatient services with speciality in memory care including a Brain Innovation Center and speech and language therapies. In-person and virtual opportunities for PT/OT/ST (cognitive communication therapy), offered for patients on a wide range of insurance, from private insurance to Medicaid. https://www.sralab.org/
Doll & Pet Therapy – patients can use a baby doll or robotic pet to reduce stress, distress and agitation and have someone to look after. For more information and to order see: https://www.alzstore.com/doll-pet-therapy-dementia-s/1516.htm
Dementia Friendly Activity Board – these are available on and Amazon and Etsy and are great to do with a caregiver or alone. For more information see: https://seniorsafetyadvice.com/activity-boards-for-dementia-patients/
Puzzles to Remember – puzzles are excellent activities for memory care patients. These puzzles are specifically created for people with Alzheimer’s disease. See for online purchasing: https://www.springbok-puzzles.com/alzheimer-s-puzzles-s/1849.htm#:~:text=Springbok%20Alzheimer%27s%20Puzzles%20Springbok%20is,individuals%20suffering%20from%20Alzheimer%27s%20disease.
Q: What's the difference between Home Care, Home Health, and Outpatient Therapies?
In-Home Care / Caregiving / Homemaker Services (non-medical order) – These terms all refer to non-medical services offered for companionship, light housework, meal prep/cooking, social engagement, and personal care for a person that needs assistance with their Activities of Daily Living or instrumental Activities of Daily Living. They may stay from 4-6 hour shifts or up to 24/7 depending on the person’s level of care needs. This service can be free, reduced cost, or private pay depending on eligibility. See above sections for these options in care.
Home Health Therapy (medical order) – HH is an insurance-covered medical order that is prescribed by the doctor, for physical therapy (PT), occupational therapy (OT), speech/cognitive therapy (ST), nursing/medication management (RN/SN), and bathing assistance (CNA services). These are often once a week for a 45 min. visit.
Outpatient Therapy (medical order) – Can go to any insurance-compatible outside vendor for physical therapy (PT), occupational therapy (OT), speech/cognitive therapy (ST). These are often once a week for a 45 min. visit.
__________________
Of note, home health and outpatient therapies cannot occur at the same time if billed under insurance. Free, donation-based clinics such as the DePaul Speech and Language Clinic do not bill insurance and therefore can be utilized concurrently.
Moreover, insurance-covered therapies require a doctor’s visit either 30 days beforehand or within 90 days afterwards. The insurance company is interested in covering for a medically necessary and recent evaluation.
6. Safety: At Home & On the Road
Memory loss can include unpredictable moments. Learn ways to be proactive and preventive with safety measures for everyone at home and on the road. A key component to memory loss, is that the person may toggle between having moments of clarity and a moment of impairment. When they are in the midst of this ‘memory glitch’, the brain may be operating from a very small size: the skillset and capacity of a very small child, in that. very moment. So the person is genuinely, at no fault of their own, potentially afraid or unable to remember how to manage the moment as if they were fully present and able. Or the short term memory loop may prevent the person from remembering the stove is on, or which pedal on the car to step, and slowed reaction time due to impaired brain processing time may increase risk of car accidents. This is why it can be good to be proactively plan ahead for personal safety and secure the living environment with the tools and devices necessary in advance.
In this section:
– Safety at Home & Wandering prevention
– Safety on the Road & Driver Evaluation
Q: What do I need to consider to be safe at home? Is there anything that can help me prepare for or notice symptoms in advance?
Consider acquiring an ID bracelet so that your care partner can be contacted in the event of an emergency, especially in case the person is lost and/or does not have access to a phone. A GPS wearable can also be explored.
http://directives.chicagopolice.org/forms/CPD-52.300.pdf
This is an example of an ID bracelet that is engraved with the care partner’s contact information. It can be obtained by your local police station.
Ask your doctor for a home safety evaluation by a home health agency. An occupational therapist is trained for this purpose.
Home safety tips:
www.nia.nih.gov/health/home-safety-checklist-alzheimers-disease
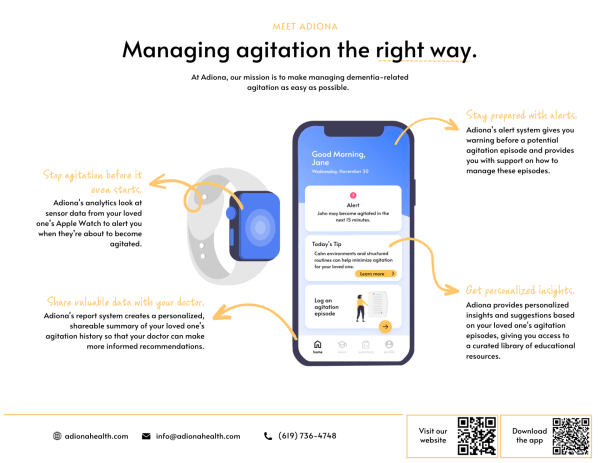
www.adionahealth.com
Sometimes it can be helpful to know when symptoms or safety concerns are arising. Adiona Health is a community partner of The Memory Center and it is an app that can be paired onto your device to detect when flare-ups and agitation might be occurring imminently. Feel free to explore!
Q: What do I need to consider to be safe on the road?
https://myaota.aota.org/driver_search or in Chicagoland at https://www.sralab.org/lifecenter/resources/listing-drivers-rehabilitation-programs-chicago-area-and-beyond
- Talking about Driving: (www.alz.org/driving)
Free home and car safety conversation guides: (www.thehartford.com/resources/mature-market-excellence/publications-on-aging)
- Learn about driving safety: www.nia.nih.gov/health/driving-safety-and-alzheimers-disease
7. Exploring Clinical Research Studies & Medical Treatment
Learn about the opportunities available to you if interested in medical treatments and participating in clinical studies contributing to research towards the cause and cure.
In this section:
– Treatment and Medications
– Research studies and Clinical trials
Q: What medications are involved in treating memory loss and dementia?
There are a variety of scenarios where we might use medications to help care for you or your loved one.
Cognitive Enhancers – These medications are used to try and slow down the progression of the symptoms of dementia.
* Cholinesterase Inhibitors – this class of medication is indicated for use in early stages of dementia and throughout the course of the disease
– Donepezil (Aricept)
– Galantamine (Razadyne)
– Rivastigmine (Exelon)
* NMDA Receptor Antagonists – this class of medication is indicated for during the moderate stage of dementia and through the later stages of the disease.
– Memantine (Namenda)
* Combination Cholinesterase Inhibitors + NMDA Receptor Antagonist
– Donepezil/memantine (Namzaric)
Anti-Depressants – Most often used to help manage symptoms of depression, anxiety, frustration, and agitation. While there are several classes of medications this is the class we generally start with unless there are contraindications.
* SSRI (Selective Serotonin Re-uptake Inhibitors)
– Sertraline( Zoloft)
– Citalopram (Celexa)
– Escitalopram (Lexapro)
Sleep Aids – these medications are anti depressants by class, but we use them often to help with sleep initiation difficulties. We avoid sleep aids such as ambient or Benadryl as they can increase confusion.
– Trazodone
– Mirtazapine (Remeron)
Anti-psychotics – These are used sparingly to help manage hallucinations, delusions, or severe agitation that can be present for some patients.
– Quetiapine (Seroquel)
– Risperidone (Risperdal)
– Olanzapine (Zyprexa)
– Brexpiprazole (Rexulti) – recently approved for control of agitation in Alzheimer’s
Drugs that directly work to remove the beta amyloid plaques of Alzheimer’s Disease – these are IV infusions, that are indicated to be used for those with confirmed Alzheimer’s Disease in the mild stage.
– Aducanumab (Aduhelm)
– Lecanemab (Leqembi)
Q: What current research studies are happening at The Memory Center?
* Agitation – An investigational drug study aimed to help patients with Alzheimer’s who experience agitation and behavioral disturbances.
* Gut Microbiome Study – An investigational study to look at the connection between the microbiome of gut and Alzheimer’s Disease in African American patients
* Social Cognition Study – An investigational study looking at social cognition and social awareness in patients with cognitive impairment and dementia.
* Capacity Study – An investigational study looking at the ability to make medical decisions independently in patients with dementia.
* New iDEAS – A national study that is giving access to Amyloid PET scan (a scan used to detect the amyloid plaques that deposit in the brain of patients with Alzheimer’s Disease) to African American and Hispanic patients who also have Medicare or Medicare Advantage Plan as their primary insurance.
* Predicting Agitation in a Patient with Alzheimer’s Disease Using an Apple Watch – This study will test a computer program we have developed to work in an Apple watch that the patient will wear. Detection of an episode of agitation before it starts will allow the caregiver to interrupt the episode and improve the patient’s overall well-being.
* Art Is…In – Art Therapy program for patients with dementia and their caregiver that is looking to better understand caregiver bond and burden.
8. Lifestyle, Wellness, & Quality of Life
Music, movement, and arts are the key to brain health and wellness. Nutrition, sleep, exercise, stress management, and social engagement are the key factors in delaying the onset and progression of memory loss, heart disease, dementia, diabetes, and stroke. Explore these opportunities out in the world and from the comfort of home.
In this section:
– Lifestyle for brain health and wellness
– Music, Movement, and Arts
– Social engagement, fitness, wellness
Q: What are the top recommended lifestyle tips for optimizing brain health and wellness? Can this apply to both patients and caregivers?
Adapted from
MensFitness | Brain Health
by Sarah Di Giuilio (via an interview with Dr. Mastrianni, The Memory Center)
The secret to good brain health is to stay healthy from head to toe. Many medical conditions can cause or promote memory decline, especially cardiovascular issues, sleep disorders, and depression. So, make sure that you are following the recommendation of your general doctor and specialists and taking your medications, as prescribed. In addition, research over the last several years has provided strong evidence that several lifestyle modifications can help to delay the onset or the progression of Alzheimer’s Disease and related dementias. We’ve listed some key things to incorporate in your daily routine, that should help ensure the best possible brain health.
1. Develop an Exercise Routine – Regular physical activity is one of the best ways to keep your brain healthy. The more you keep the body, as well as the mind, engaged and active, the better both will work together. A considerable amount of research suggests regular exercise can improve cognition and delay the development of dementia. Current guidelines recommend at least 150 minutes of moderate-to-intense aerobic activity each week. Although a cardio work out such as running, brisk walking, or using the treadmill, stationary bike, or elliptical has the greatest evidence to benefit the brain, newer studies also suggest some degree of muscle-building activity can help. We recommend starting with a cardio workout, just a few minutes a day for the first week and slowly building up the time spent each day until you reach the goal of 30 minutes or more per day.
2. Get Your Sleep – When your body feels tired from the lack of shut-eye, your brain suffers. It’s not able to concentrate and focus as well as it does when it’s rested. Studies show that sleep not only allows your brain to rejuvenate, it has important biological functions that impact memory and risk to, or progression of, dementia. During sleep, detrimental proteins that accumulate in Alzheimer’s disease are cleared away while the brain actually works to strengthen memories of the day. Sleep duration should be between 7 and 9 hours, as studies suggest that sleeping shorter or longer can be detrimental to your cognitive functioning and the progression of Alzheimer’s Disease. And if you’re feeling extremely drowsy during the day and can lie down, strategic 10- or 20-minute naps can improve overall focus. But sleeping for longer than 1 hour during the day isn’t a great idea, as this could interfere with your nighttime sleep schedule. If you exercise daily, that will help you sleep at night! If you have a lung disease, or sleep apnea, make sure you take good care of those conditions, as they may impair oxygen delivery to your brain, which is critical for the brain to function optimally.
3. Eat a Healthy Diet – The good fats found in fish, as well as some nuts may help to protect your brain cells and keep them functioning at their peak. Some studies have shown that omega-3 fatty acids, in particular, may improve cardiovascular function, which in turn improves brain function because what’s good for the heart is good for the brain! However, not all studies show consistent results – it is thought that getting the omega-3 from the source rather than from pills, which is done in such studies, may be best. In fact, dietary studies have found that people who eat at least one seafood meal a week (regardless of whether those fish have fins or shells!) have less Alzheimer’s Disease pathological changes in their brain at death. Multiple studies repeatedly show that a Mediterranean diet rich in fish, fruits, and vegetables increases longevity and delays the development of cognitive decline. So fish really is good brain food!
4. Get Your Vitamins Insufficiencies in certain B vitamins, as well as vitamin D and folic acid, worsen brain function in the short term—and could even mimic signs of dementia. Eating a well-balanced diet that includes fruits, vegetables, and low-fat dairy provides most people the daily allotment of vitamins they need. If you opt for a multivitamin, read the label and look for one with at least 100% of your recommended daily allowance of vitamin E, vitamin D, B-complex vitamins (B-1, B-6, and B-12), and folic acid. Don’t overdo supplements! Most supplements are promoted by the companies that make them or “testimonials” on the internet from people who claim that they have “noticed an incredible improvement in memory” after taking them – don’t trust these testimonials, as they are not supported by well-designed clinical trials that rigorously test products and many such online “testimonials” might actually be generated or supported by the companies that make the supplements. In addition, high doses of some supplements might actually be harmful to some patients, depending on their medical condition and other medications they are taking. The best advice is to, always ask your doctor whether a supplement is appropriate.
5. Do: Stay Social
Avoid isolating yourself. Return a phone call and make plans. Stay engaged in social activities. Social interactions stimulate the mind, heighten brain activity, and present new problems for the brain to solve—which is one of the best ways to keep it in shape. In the long run, real-life problem-solving improves memory and helps cognitive functioning even more than word games and memory exercises.
6. Don’t: Stress Out
We know—easier said than done. While some stress and anxiety may help motivate you to meet an approaching deadline, taking on too much backfires and prevents the brain from absorbing information as efficiently as it should. The long-term effects of stress hormones like cortisol can actually cause damage to brain cells, possibly affecting the hippocampus especially (the brain region that allows us to make memories). In fact, exercise has been shown to build up the hippocampus – that’s why the first step to good brain health is exercise!
More from the Alzheimer’s Association on lifestyle for optimal brain health: https://www.alz.org/help-support/brain_health/stay_mentally_and_socially_active
Q: What virtual/at-home social engagement, fitness, and wellness options are available?
Social Engagement / Music / Movement / Arts at home:
Here are some virtual activities you can do from the comfort of home, yourself or with someone who can help him be active when you have backup care at home:
AARP Virtual Community Center – AARP Virtual Community Center – Find Free Online Events – AARP
COVIA.org – Front Porch – Well Connected – Front Porch | Front Porch (covia.org)
NSSC.org – North Shore Senior Center Virtual Activities – Virtual Activities (nssc.org)
ZinniaTV.com – Zinnia TV
Memory Lane TV – https://www.memory-lane.tv/families
Memory Cafe Directory – Memory Cafe Directory – Dementia-Friendly Outings for All!
50 Activities – 50 Activities | Alzheimer’s Association
The Smithsonian Channel I’m hearing also has some excellent visuals of “traveling around the world”
Sounds Good Choir + the Good Memories Choir – Good Memories Choir – Sounds Good! Choir (soundsgoodchoir.org) – virtual opportunity for the patient and care partner
Dementia Map – comprehensive listing of national events and activities in dementia care
Q: What in-person social engagement, fitness, wellness options are available?
Healthy Aging Communities in Chicago
Chicago Hyde Park Village: (Hyde Park) South Side neighborhoods (www.chpv.org)
Lincoln Park Village: (Lincoln Park) Edgewater to the Chicago River (https://thevillagechicago.org/)
North Shore Village: (Evanston, Wilmette, Skokie, Glenview, Winnetka) (www.northshore-village.org)
SkylineVillage Chicago: (high-rise section) North Avenue to the Loop (www.skylinevillagechicago.org)
Arts, Music, and Movement (For better brain health & enhanced quality of life)
Alive Inside: Documentary on music and memory (also streaming on Netflix) (www.aliveinside.us)
GoldMindArts: Weekly in-home art sessions with patient and caregiver exclusively for Memory Center patients (www.goldmindarts.com)
Chicago Dance Therapy: (www.chicagodancetherapy.com) | Email iladtachapter@gmail.com for referral. This practice offers counseling with a body-centered approach focused on connecting mind, body, and spirit
Old Town School of Folk Music: https://www.oldtownschool.org/classes/adults/
Video Family Biographies: Preserve your family story (www.videofamilybiographies.com) StoryCorps: Interview your loved one about their life (storycorps.org/discover/memory-loss-initiative/)
MyAlzheimers: Building the World’s Largest Collection of Alzheimer’s Stories (www.myalzheimers.net)
Sounds Good Choir: Join your local chorale with other older adults who love to sing! (https://soundsgoodchoir.org/) The Good Memories choir serves people with early-stage memory loss and their care partners.
Greater Chicago Music Therapy: Offering group and individual music therapy sessions. Contact Mia Iliopoulos, music therapist and dementia practitioner, (847) 863-0234, www.greaterchicagomusictherapy.com.
Musical Bridges to Memory: This program is run through the Institute for Therapy Through the Arts, currently offered online and at specific memory-care facilities. https://itachicago.org/musical-bridges-to-memory/ or contact Amanda Ziemba, 847-448-8332 to enroll.
Songs by Heart: Live music performances at residential care facilities (www.songsbyheart.org)
TimeSlips: An organization focused on creative engagement and resources for patients and caregivers. https://www.timeslips.org/
Music & Memory: An organization dedicated to utilizing music with memory care patients to improve mood and quality of life. Create a personalized playlist to play at home: https://musicandmemory.org/resources/#loved-one
Tales & Travel Memories is an innovative book and reading library program that provides services directly to people diagnosed with Alzheimer’s Disease and related dementias through storytelling videos available online and in person programs in the Gail Borden Public Library District and assisted living facilities in Elgin, IL: http://talesandtravelmemories.com/memory-cafes/; http://talesandtravelmemories.com/about/
Virtual Programming:
ZinniaTV: A dedicated TV station for patients experiencing memory loss. Patients and caregivers can explore many different channels including “nature, places, animals, activities”. 14-day free trial followed by subscription service: https://www.zinniatv.com/
AARP: https://local.aarp.org/virtual-community-center
Covia Well-Connected: https://covia.org/programs/well-connected/
North Shore Senior Center: https://nssc.augusoft.net/index.cfm?fuseaction=1010
Socialization / Fitness Opportunities
Illinois Department on Aging Adult Day Centers and Homemaker Services (illinois.gov/aging)
Memory Cafes and RAILS Library Programs social gatherings hosted by local libraries and agencies (For memory cafes for patient and caregiver check out https://www.memorycafedirectory.com/state-directories/; https://www.memorycafedirectory.com/memory-cafes-in-illinois/ ; https://www.memorycafedirectory.com/memory-cafes-in-indiana/)
Chicago Senior Centers (Chicago Department of Aging) https://www.cityofchicago.org/city/en/depts/fss/provdrs/senior/svcs/regional_senior_centers.html
Atlas Center (aka www.79thstreetseniors.com)
South Side YMCA (http://www.ymcachicago.org/southside/)
Nash Community Center Natatorium (Park District) (www.chicagoparkdistrict.com)
Harris Center Field House (Park District) (www.chicagoparkdistrict.com)
Kroc Center (http://www.kroccenterchicago.com/)
Mathers More Than a Cafe: https://www.mather.com/neighborhood-programs
Silver Sneakers – (https://www.silversneakers.com/)
University of Chicago Community Fitness Program – (https://www.uchicagomedicine.org/about-us/community/programs-services) 773-702-5600
Galter Life Center – Medical Fitness Center (http://galterlifecenter.org/) 773-993-1232
CJE Senior Life – Enhancing lives of older adults with life enrichment programs (www.cje.net)
Center for Life & Learning – (http://www.fourthchurch.org/cll/index.html)
Memory Cafe Directory – Memory Cafe Directory – Dementia-Friendly Outings for All!
www.nadsa.org – Explore your local Adult Day center
Chicago area listing of local senior centers – https://www.chicago.gov/city/en/depts/fss/provdrs/senior/svcs/regional_senior_centers.html
To inquire about your local senior center and other programs, resources, and caregiver support services available to you, visit:
www.ilaging.illinois.gov – Department on Aging – City of Chicago
www.AgeOptions.org – Suburban Cook County
www.AgeGuide.org – Collar Counties (DuPage, Grundy, Kane, Kankakee, Kendall, Lake, McHenry and Will)
www.eldercare.gov – National Website for your local Area Agency on Aging
9. Living Alone
Follow these tips for optimal safety and care while living alone. Know when to get additional support for optimal safety and well being.
In this section:
– Tips for managing care while living alone
Q: What do I need to consider if I live alone?
Alzheimer’s Society – https://www.alzheimers.org.uk/get-support/staying-independent/living-alone
National Institute on Aging – https://www.nia.nih.gov/health/tips-living-alone-early-stage-dementia
Little Brothers Friends of the Elderly | Chicago – https://lbfechicago.org/ – Specializing in visitation, vacations, and creative programming year-round, including holidays, for isolated elderly that qualify based on little to no local network. Call to explore eligibility
Getting someone to represent your wishes and secure your finances – Consult an elder law attorney to plan out your care/finances (www.naela.org), complete your advance directives (select a Power of Attorney), and make sure your bills are on autopay or in the care of a trusted person or entity that can assist, like www.mypersonalbookkeeper.com.
10. For those who are working
Explore this section for questions about disability, early retirement, special benefits, and adjusting your workplace environment with accommodations
In this section:
– Making adjustments/accommodations at work
– Going on leave (FMLA)
– Applying for Disability (short term, long term, Social Security [SSDI])
Q: What do I need to consider if I'm still working?
Making adjustments/accommodations at work – In case your condition is making it challenging to complete your tasks, first consider adjusting your workload, hours, or nature of your position. If needed, talk to your employer or the Human Resources department to discuss any changes you would like to make at work. The HR department is supposed to be a confidential source of guidance. Consulting with a disability and elder law attorney can assist in this regard as well (National Academy of Elder Law Attorneys, www.naela.org).
Social Security Disability income and Medicare – You may qualify for Social Security Disability Benefits sooner if you have a diagnosis on the Compassionate Allowances List. Visit www.ssa.gov/compassionateallowances to double check if your diagnosis is listed here. Schedule your interview with Social Security (800-772-1213) and mention the Compassionate Allowance diagnosis. Those on this list are more likely to get fast-tracked approval for disability benefits, and you may be entitled to receive Medicare benefits after 24 months of payment (a.k.a. you can get Medicare after 2 years of Social Security disability income).
PRO-TIP: You often do not have to pay for an attorney to help you apply for disability. You will be assigned your own personalized free case adjudicator in the SSA office to handle your case. Be sure to give them your doctors’ name, phone number, and address so that the SSA can receive medical documentation as proof of your diagnosis. Your case will not be processed until all materials are received, so stay in contact with your medical providers and your case adjudicator to ensure timely submission.
FMLA Leave – Memory loss can make work tough for yourself and/or your care partner – If either of you need to take some time off work, either due to your condition or to receive assistance for your care (e.g. getting to/from medical appointments, help at home for your daily activities, they can request up to 12 weeks of unpaid leave from the Family Medical Leave Act (FMLA)* with a reduced work schedule, intermittent or continuous leave. Send it to your primary care physician or to our clinic to process paperwork for approval by your employer.
*Employees are eligible for leave if they have worked for their employer at least 12 months, at least 1,250 hours over the past 12 months, and work at a location where the company employs 50 or more employees within 75 miles. -U.S. Department of Labor
11. For those under 65 (Young Onset)
Experiencing cognitive impairment or a young onset dementia (diagnosis under age 65) comes with a unique set of challenges. We understand that the lives of working professionals with growing families and dreams of travel and retirement life change suddenly, and it’s vital to find peer support and resources along this journey.
In this section:
– Coping and adjusting to the unique challenges of Young Onset diagnoses
Q: Where is there support for those diagnosed under age 65?
Those experiencing younger onset Alzheimer’s or other related dementia diagnosis encounter unique challenges that impact the entire family. One of the most helpful things you can do is connect with others that have a common experience.
Some of the most common concerns are finding support for the children/youth, identifying ways to stretch one’s dollar for single income household’s on an unexpectedly reduced budget, and finding adequate, age-appropriate care.
How and when do I Share the news? – Sharing a Dementia Diagnosis with Family and Friends – a guide presented by Alzheimer’s Texas, for Alzheimer’s Disease and related disorders
Lorenzo’s House – www.lorenzoshouse.org – Lorenzo’s House is a budding non-profit with global monthly virtual support and programming available for youth, care partners, and patients diagnosed with Alzheimer’s Disease and other related dementias. Lorenzo was a dear patient here at The Memory Center, and his wife Diana retired from her career in education to start Lorenzo’s House in response to the care and connection gap for younger onset families. (Global virtual support for care partners as well as age-specific youth/young adults with parent diagnosed; Music, Movement, and Memory program open to those diagnosed and with their care partners in Chicagoland)
Without Warning – www.withoutwarning.net – Without Warning offers monthly virtual support for early, middle, late stages (United States)
Alzheimer’s Association – https://www.alz.org/help-support/i-have-alz/younger-onset – Find local support anywhere in the country for younger onset Alzheimer’s Disease and other related dementias (United States)
Paul’s Club – https://paulsclub.weebly.com/ (Vancouver, Canada)
Dementia Action Alliance – www.daanow.org (a ‘for us, by us’ community)
Dementia UK – https://www.dementiauk.org/about-dementia/young-onset-dementia/young-onset-dementia-resources/
Young Dementia Network – https://www.youngdementianetwork.org/ – (hosted by Dementia UK); resources: https://www.youngdementianetwork.org/resources/
Younger People With Dementia – https://www.ypwd.info/
Rainbows for all Children – https://rainbows.org/resources/chronic-illness/ – Resources for children age 8-18 managing chronic illness in the family
Pickles – https://www.picklesgroup.org/learn – This organization is designed for kids managing cancer diagnoses, however this particular link is rich with resources for supporting children through all facets of life when a parent is diagnosed with a chronic condition
Young Timers (for those with confirmed familial/hereditary young onset dementia) – https://www.youngtimers.org/aboutus – a patient-led organization, founded by a group of early onset familial Alzheimer’s disease (EOFAD) family members and other stakeholders to help better address the needs of individuals and families affected by this young hereditary dementia.
Additional Recommendations:
– Awareness Cards – For young onset dementia, interacting with others in the world may be challenging, as they expect a certain encounter. Since we are able to detect body language and facial expression quite easily, it can be helpful to reduce difficult exchanges or awkward glances that don’t feel good on the receiving end, by having an awareness card at the ready. Here are some examples from the Alzheimer’s Association and The Association for Frontotemporal Degeneration, or you can make your own as well, similar to JAM Cards (‘Just A Minute (of patience) Thank you’). They can help elicit immediate patience and compassion, let alone a warm, understanding facial expression that invites inclusivity, not rejection.
– Advance Planning – Refer to #4 above for advance care planning. It may especially be helpful to tap into resources that allow you to stretch your dollar and creatively plan alternate funding sources for care.
– Disability income benefits – Remember to check if you qualify for Social Security and Medicare benefits early through the Compassionate Allowances List of special qualifying diagnoses that fast-track the process. See #10 for more information if you are still working.
– Personal Assistant / Care attendant at home – For those under age 60, consider applying for DHS Home Services Program (you do not have to be on Medicaid for this program) and for those 60 and over, can benefit from your local area’s Aging and Disability Resource Center (ADRC) via www.eldercare.gov to learn what in-home, adult day, and caregiver support resource you have in your zip code.
– In-home care and adult day recreation programs – Some people seek neighbors and retired nurses to assist with lower cost hourly rates of care, such as through www.nextdoor.com or www.care.com in addition to utilizing adult day centers through www.nadsa.org or www.communityresourcefinder.org. Ask your social worker for a list of preferred providers who can assist with subsidized, low-cost, or private pay caregiving.
– Financial Planning – For long-term care financing, consider reverse mortgage, consulting with a disability and elder law attorney (www.naela.org). Check with your life insurance policy in case it has a clause for long-term residential care.
12. How can we help the cause?
Would you like to help raise awareness in your local neighborhood or advocate for the national cause?
In this section:
– Local and national opportunities to educate others, raise awareness, get involved, volunteer, and support
Q: How can I help my local neighborhood be more 'dementia friendly'?
www.ilbrainhealth.org – Explore all the dementia care initiatives happening throughout the state of IL
www.dementiafriendsusa.org – A national initiative to raise awareness by viewing short videos and sharing. Become a ‘Dementia Friend’ and spread the word!
www.dfamerica.org – Dementia Friendly America is a national initiative to enhance dementia awareness in every sector (storefront, library, dining, medical, school, etc.). To find your local Dementia Friendly neighborhood, visit this link. If in IL, visit www.ilbrainhealth.org above.
www.chpv.org/dfhp – Dementia Friendly Hyde Park (local to The Memory Center)
Q: What advocacy organizations exist to advance the cause?
Grief and loss support can happen now
Memory loss and dementia comes with many types of losses: loss of independence, loss of the partner or parent you once knew, both sides are grieving, holding onto hope while letting go all at once. Learn more here.
In this section:
– Coping through the many types of loss
– Grief support
Q: How do I deal with tough feelings of loss? Where can I get support?
With memory loss comes many forms of losses.
For the person diagnosed, it’s a loss of identity, independence, abilities, and hopes for their future.
For the care partner, spouse, or young/adult child, it’s a loss of the person they once knew, “She’s still here, but I miss her,” is a common phrase. And in assuming the identity of caregiver, it’s also a loss of themselves and their own hopes and dreams in life.
Finding ways to make meaning of these progressive losses is vital to everyone’s quality of life. Feel free to seek counseling at any time in your journey to make sense of it all. So that you can optimize the time you have.
_______________
Lightways – www.lightways.com –
- Short term grief counseling – virtual or phone and in person at the office – free. No insurance. Death of loved one.
- Support groups – spousal partner loss, child loss, parenting while grieving (online); Education workshops (no counseling but yes to class)
- Grief camp – age 7-13
Center for Grief Recovery – www.griefcounselor.org
The Dougy Center – www.dougy.org
What’s Your Grief? Grief Support for the Rest of Us – www.whatsyourgrief.com
Refuge in Grief: It’s OK to not be OK – www.refugeingrief.com
National Alliance for Children’s Grief – www.nacg.org
For young onset with children: Ask your local provider for a recommended Child Life Specialist. They are seasoned in preparing for and counseling children through the grief process, including what to expect, how to prepare, what can be done now and beyond, for healthy coping and meaning-making of the loss. Given that the journey in dementia care has an unpredictable timeline, it can be helpful to connect them with support early on so they know how to manage the progressive changes along the way.
Rainbows for all Children – https://rainbows.org/resources/chronic-illness/ – Resources for children age 8-18 managing chronic illness in the family
Pickles – https://www.picklesgroup.org/learn – This organization is designed for kids managing cancer diagnoses, however this particular link is rich with resources for supporting children through all facets of life when a parent is diagnosed with a chronic condition
Additional Counseling Options
–Family healthcare counseling (www.ccfhchicago.org) 312-372-4731
–Counseling (www.inhomecounselingforseniors.com) 888-903-5604
–Mental health resource/help 312-563-0445 (www.namichicago.org)
-Chicago Center for Cognitive Wellness: Therapists with expertise in memory care and memory loss diagnoses. Dr. Sherrie All is a clinical neurorehabilitation psychologist and brain health expert. http://cogwellness.com/, 773-345-3495, Edgewater and Loop office locations.
– For peer-to-peer support: Dementia Action Alliance is support for those with dementia by those with dementia. www.daanow.org
- Ask your social worker, a Certified Dementia Communication Specialist for a detailed list of suggested counseling services and providers.
Where else can I receive individualized support and resources for care planning through this journey?
In addition to the wealth of resources you have above, as well as the local and national organization that supports your specific diagnosis, here are some options for further care planning guidance, including culturally relevant and LGBTQ+ resources. You are not alone!
In this section:
– Care Planning Guides and Toolkits
– Care Planning Consultations (virtual and in-person)
Q: How else can I find comprehensive care planning support and guidance?
– Care Planning Guides:
(1) Our team members have contributed to the development and creation of this comprehensive care planning resource guide: ‘Centering Our Values’ curated by SHARE Network Chicago, our very own HRSA grant funded initiative within the UChicago Medicine Geriatrics and Palliative Care Section. Visit here: https://centeringourvalues.org/
(2) ‘Pathways to Well-Being’ – https://daanow.org/pathways-to-well-being-with-dementia/
(3) Dementia Unplugged – View this series of videos from the Dementia Society of America – https://www.youtube.com/playlist?list=PLoyKaLxoKOcWxh-uIUtAvid4avZ5d31xj
– Care Planning Consultations:
(1) Knight Family Foundation – 90 min free care planning session (virtual or in-person) – https://www.alz.org/help-support/resources/knight-family-dementia-care-coordination-initiativ – Visit the website link or call 800-272-3900 and mention that you would like to schedule a Knight Family Foundation care consultation.
(2) If you are an established Memory Center patient, schedule a consultation with the licensed clinical social worker by contacting the clinic or leaving a message on MyChart, and the nurse will direct your message accordingly.
If you are not yet an established patient and would like to be seen by our interdisciplinary team for a medical diagnosis, treatment, and ongoing care in the clinic, patients of any age can contact (773) 702-6222 to schedule an appointment with one of our Memory Center providers. (For those that are over age 65 with Medicare and interested in being seen at our South Shore location for The Memory Center, contact (773) 702-8840 for scheduling. (Click here to view our locations)
Q: Where can I find culturally relevant support?
– Coalition for Limited English Speaking Elderly – www.clese.org
– Chinese American Service League Alzheimer’s Program – https://www.caslservice.org/alzheimers/
– La BROCHA Chicago – https://www.facebook.com/LaBrochaChicago/ and https://www.instagram.com/_labrocha/?hl=en
– Latino Alzheimer’s and Memory Disorders Alliance – https://www.latinoalzheimersalliance.org/care-caregiver-programs
– Centering our Values – A comprehensive care planning site and PDF guide, available for use by all populations, and especially with African American communities in mind – https://centeringourvalues.org/
– CJE Senior Life: Jewish Values for Positive Aging – https://www.cje.net/
– Japanese American Service Committee – https://www.jasc-chicago.org/community-services/for-seniors/adult-day-services/#:~:text=The%20rate%20is%20%2475%20per,check%20out%20this%20wonderful%20program.
– Illinois Aging Together – https://illinoisagingtogether.org/about/supporters/
Q: Where can I find LGBTQ+ resources?
– SAGE: Advocacy and Services for LGBTQ+ Elders – https://www.sageusa.org/
– Alzheimer’s Association LGBTQ+ Community Resources for Dementia – https://www.alz.org/help-support/resources/alzheimers-and-dementia-resources-for-lgbtq-commun
– Howard Brown Health – https://howardbrown.org/aging-services-community-resources/
– National Resource Center on LGBTQ+ Aging – https://www.lgbtagingcenter.org/resources/resources.cfm?st=IL
If you are not yet an established patient and would like to be seen by our interdisciplinary team for a medical diagnosis, treatment, and ongoing care in the clinic, patients of any age can contact (773) 702-6222 to schedule an appointment with one of our Memory Center providers at our Hyde Park location. (For those that are over age 65 with Medicare and interested in being seen at our South Shore location for The Memory Center, contact (773) 702-8840 for scheduling. (Click here to view our locations). Otherwise if you are simply visiting this site as a guest, you are welcome to explore!
The resources, content, and links above do not necessarily represent the views nor endorsement from UChicago Medicine or any of its affiliates. The views expressed also do not replace or represent current programming nor professional medical or counseling. Feel free to explore the resources freely to clarify the details and availability of programs since they may be subject to change over time. If needed, consult a licensed clinician or medical professional to confirm which resources are relevant and compatible for your use.
